Part 1 of this series introduced the concept of hybrid antibodies: naturally occurring molecules comprised of the binding domain of a receptor fused onto the scaffold of an antibody.1 These strange proteins challenged our understanding of how antibodies are built, and much remains to be understood about them. When first reported in 2016, the LAIR1 hybrids (i.e., antibodies with LAIR1 insertions that conferred reactivity to malaria parasites) were the only type known to exist with certainty. However, there was no clear reason why other hybrids couldn’t exist—and so the search continued.
Beyond LAIR1
The discovery of hybrid antibodies was so unexpected that the researchers who first reported them probed both their origin and function meticulously.1 One likely candidate for these insertions was the RAG (recombination-activating genes) machinery, which normally separates, shuffles and rejoins DNA segments during V(D)J recombination.2 However, RAG works in a “cut-and-paste” mode, meaning that if it were responsible for producing LAIR1-hybrid antibodies, the cells should be missing part of their LAIR1 gene. Upon sequencing this region of DNA, scientists were surprised to find the LAIR1 gene fully intact.1 This implied that the creation of the hybrid genes involved a template-directed mechanism, copying parts of LAIR1 without harming it. As RAG cannot perform such duplications, the machinery responsible for hybrid antibody generation remains a mystery.2
Investigators also wanted to find out if the hybrid anti-malaria antibodies had functional activity. Although they did not interfere with parasite growth, they were able to induce agglutination (i.e., sticking infected cells together) and opsonization (i.e., coating and ‘tagging’ infected cells to be ingested by immune cells) in lab cultures of malaria.1 When the inserted LAIR1 domain was artificially removed, the hybrid antibodies lost all malaria reactivity, indicating that binding was mediated solely via the LAIR1 insert. 1 The reason for this became clear when a detailed molecular structure of one of these antibodies was revealed: the LAIR1 insert ended up perched perfectly over the antibody’s ‘prongs’, occluding the critical protein loops known as complementarity determining regions (CDRs) that are normally responsible for binding.3
Importantly, neither the generation of the hybrid antibody gene nor its three-dimensional structure seemed to rely crucially on any feature specific to LAIR1—raising the possibility that other hybrid antibodies could exist. Despite intensive efforts, it took years before the next members of the family were found: the LILRB1 hybrids.4
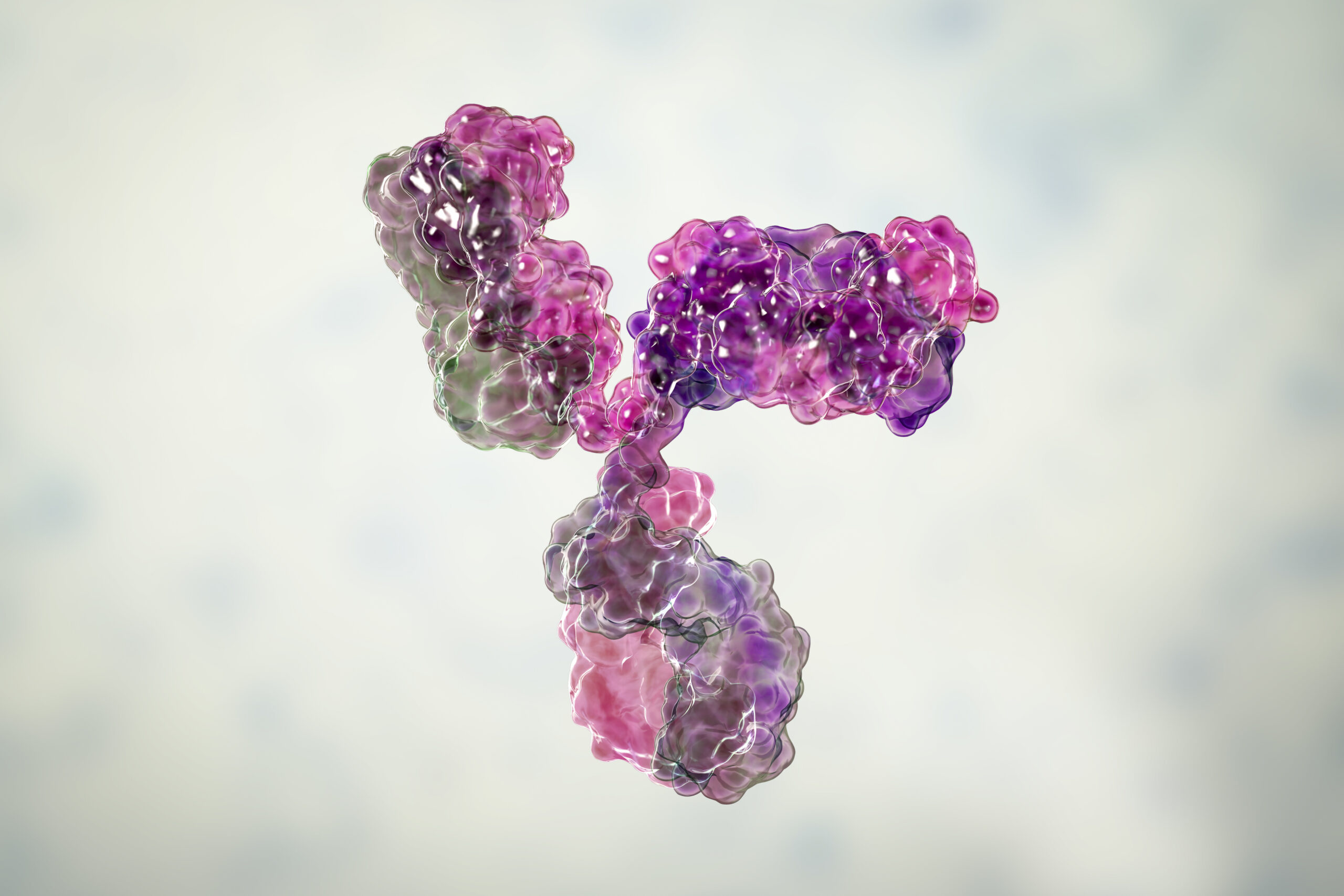
Similar to the LAIR1 hybrids, these antibodies bore a large insert from an unrelated receptor (LILRB1; normally involved in self-recognition), which enabled them to react broadly with malaria-infected cells.4 However, the architecture of these newly discovered molecules was very different from the LAIR1 hybrids: rather than having the receptor inserted on top of the CDR loops, the LILRB1 inserts extended out from the hinge just below the apical domains (termed an “elbow insertion”) (Figure 1).4 Curiously, although the CDR loops were not blocked by the insert as they are in LAIR1 hybrids, binding was still mediated solely by the domains of the inserted receptor with no contribution from the antibody.4 This suggested that the location of the inserts was not important for their function, as long as the hybrid antibody retained structural integrity and maintained its ability to bind its parasite target.
Both the LAIR1 and LILRB1 hybrids were first reported in the context of malaria infections.1,4 But it remained puzzling why reports of other hybrid antibodies weren’t emerging outside of the field of malaria—after all, we now knew exactly what to look for.

Figure 1. Antibody schematics. Graphical depictions of (a) a conventional antibody, (b) a LAIR1 hybrid antibody, and (c) two different LILRB1 hybrid antibodies. In (b), the inserted LAIR1 domain (shown in red) is located atop the variable regions while in (c) the LILRB1 domains (shown in purple) protrude out of the “elbow” of the antibody.
LAIR1, leukocyte-associated immunoglobulin-like receptor 1; LILRB1, leukocyte immunoglobulin-like receptor subfamily B member 1.
Beyond malaria
Our bodies are constantly producing new, unique antibodies at a staggering rate of 5.7×109 different types per day.* This means that, just in the time spent reading this sentence, almost 367,000 new antibodies will have been produced in yours.† These estimates were originally assumed to refer entirely to conventional antibodies, but the advent of hybrid antibodies led to an obvious question: what proportion of our antibody pool did these new molecules make up?
To answer this, researchers began profiling antibody transcripts (i.e., copies of antibody genes that have been fully assembled) from many different people.5 Much to their surprise, inserted genetic elements were found in 80% of European and African individuals. In addition, this frequency was not impacted by prior exposure to malaria.5 So, what do these hybrid antibodies bind to, and why hadn’t they been detected long ago if they were so prevalent? It turns out that not every recombined antibody gene leads to meaningful levels of an actual antibody. The first requirement is for the inserted DNA sequence to avoid disrupting the integrity of the antibody genes. Of the detected inserts, only 10% were ‘in frame’ (i.e., inserted with correct orientation and spacing to preserve the continuous protein-coding sequence).5
Second, since inserting a sequence that would confer reactivity to a pathogen is likely to be a rare event, selection of that antibody to be produced probably also requires constant stimulation—for example, a chronic malaria infection.5 What that means is that, while the mechanism that introduces inserts into antibodies is prolific, and apparently active in most people, it very rarely ends up generating physiologically useful antibody proteins outside of specific scenarios. While it is all but certain that many more hybrid antibodies exist, it might only be in the context of chronic infectious diseases that we will discover further members of the family.
Why do we need hybrid antibodies?
RAG, the conventional machinery that controls the generation of antibody uniqueness, is an ancient system, likely emerging some 500 million years ago in early vertebrates.6 As far as we know, the majority of antibodies important for fighting many of our diseases and conditions are created by RAG, which begs the question: why do hybrid antibodies exist at all? Do they play any role in human health other than in specific cases of long-term infections?
We do not know the answers to these questions yet. It might be that hybrids are a useful shortcut for the immune system to take when conditions allow, but are otherwise too risky to produce. Inserting DNA fragments that come from far away involves genetic shuffling processes that are associated with certain kinds of cancer.7 However, that doesn’t mean they can’t be beneficial to us.
Are hybrids better or worse than conventional antibodies in terms of function? Generating target-specific proteins in the lab is notoriously difficult, so is it conceivable that hybrid antibodies could be designed artificially to bind therapeutically relevant targets in new ways?8 Join us for Part 3 to explore the role of hybrids in antibody engineering.
Scientific Group has extensive experience of working in immunology, including dermatology, rheumatology, gastroenterology, and oncology. If you’d like to find out more, or are looking for expert agency support in this therapy area, please contact alejandro.potes@wearescientific.com
*Clonal antibody generation rate (5.7×109 clones per day) was estimated by multiplying the mean B cell production rate (1.9% daily proliferation) with the mean number of B cells in an adult (3×1011 cells), assuming each B cell gives rise to a single and unique antibody clone.9–11
†This value was calculated based on the clonal antibody generation rate and an average reading speed of 238 words per minute, giving a value of 16,660 antibody clones generated per word read.12
References
- Tan J et al. A LAIR1 insertion generates broadly reactive antibodies against malaria variant antigens. Nature. 2016;529(7584):105–9.
- Roth DB. V(D)J Recombination: Mechanism, Errors, and Fidelity. Microbiol Spectr. 2014;2(6).
- Hsieh FL, Higgins MK. The structure of a LAIR1-containing human antibody reveals a novel mechanism of antigen recognition. Elife. 2017;6.
- Chen Y et al. Structural basis of malaria RIFIN binding by LILRB1-containing antibodies. Nature. 2021;592(7855):639.
- Lebedin M et al. Different classes of genomic inserts contribute to human antibody diversity. Proc Natl Acad Sci USA. 2022;119(36).
- Hsu E. V(D)J recombination: of mice and sharks. Adv Exp Med Biol. 2009;650:166–79.
- Alt FW et al. Mechanisms of Programmed DNA Lesions and Genomic Instability in the Immune System. Cell. 2013;152(3):417.
- Cao L et al. Design of protein-binding proteins from the target structure alone. Nature. 2022;605(7910):551–60.
- Macallan DC et al. B-cell kinetics in humans: rapid turnover of peripheral blood memory cells. Blood. 2005;105(9):3633–40.
- Sender R et al. The total mass, number, and distribution of immune cells in the human body. Proc Natl Acad Sci USA. 2023;120(44):e2308511120.
- Alberts B et al. Molecular Biology of the Cell. 4th ed. Garland Science; 2002.
- Brysbaert M. How many words do we read per minute? A review and meta-analysis of reading rate. J Mem Lang. 2019;109:104047.